The model for Healthcare delivery in the United States has evolved from a paternalistic, volume based approach through an era of shared responsibility and now into a consumer driven value based model. To remain competitive in today’s healthcare market, hospitals and providers must strive for patient safety and satisfaction in the delivery of patient care. Creating and maintaining a safe environment is foundational to patient safety.
The model for Healthcare delivery in the United States has evolved from a paternalistic, volume based approach through an era of shared responsibility and now into a consumer driven value based model. To remain competitive in today’s healthcare market, hospitals and providers must strive for patient safety and satisfaction in the delivery of patient care. Creating and maintaining a safe environment is foundational to patient safety.
Writing in the Healinghealth.com blog, Susan Mazer writes about the importance of a clean and safe hospital environment. She notes “The patient environment of care plays a vital role in the discipline of patient safety for every hospital. Demonstrating that the hospital is a safe place for patients and for those that work there should be of the utmost importance for all health care personnel.” She goes on to list 5 steps for improving patient safety by improving the environment. Below, are the 5 points from the original article modified to the anesthesia environment.
- Remove Equipment from Public areas: As anesthetists, we are well aware of equipment that is stored in the hallways . Not only does this extra equipment block the walkways, but it also increases the risk of tripping and makes cleaning more difficult. Work with others in the OR suite to return excess equipment to the proper place and keep the halls free from clutter
- Minimize clutter within the operating room: Extra monitors, pumps, warmers etc stored behind the anesthesia machine or cart limits your ability to move within the room and increases the risk for tripping. Excess equipment also reduces your ability to clean between cases and increases the infection risk. As above, return all excess equipment to the proper place before starting your case.
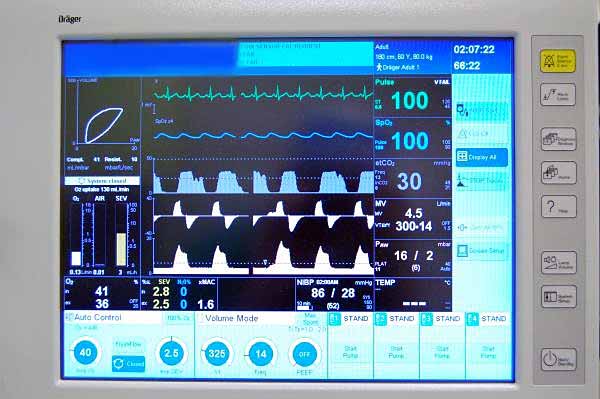
- Organize your cart and machine work space: Everything needs to be seen and immediately available before starting the case. Organize your work space the same way for every case so you know where to look for any drug or piece of equipment. Have a place for drugs, airway equipment and paperwork so that each is readily available.
- Inspect your workspace and monitors for cleanliness: Don’t rely on housekeeping to get it right. Look for residual blood or body fluids on your equipment and re-clean them if necessary. Patients expect and deserve a clean environment that protects them from infection
- Minimize auditory clutter: OK, music is great but it’s not the main event in the operating room. Patient centered care requires the provider to be able to hear monitors, alarms and be able to communicate with the surgeon. Keep the noise low and develop a “sterile cockpit” attitude during induction and emergence.
Developing and maintaining a safe environment involves more than the anesthetist. The entire operating room crew must be on board and work together to ensure a clean, clutter free environment that promotes patient safety.