 Postoperative cognitive dysfunction (POCD) is a common complication after major surgery with general anaesthesia in the elderly. Due to the increase of average life expectancy, an increasing number of elderly patients undergo surgery. Following surgery, elderly patients may exhibit cognitive changes.
Postoperative cognitive dysfunction (POCD) is a common complication after major surgery with general anaesthesia in the elderly. Due to the increase of average life expectancy, an increasing number of elderly patients undergo surgery. Following surgery, elderly patients may exhibit cognitive changes.
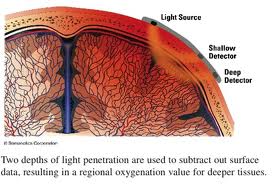
Anesthesia researchers have speculated that single lung ventilation places an elderly patient at increased risk for reduced cerebral oxygenation and also speculate that reduced cerebral oxygenation correlates with postoperative cognitive dysfunction. Two recent studies have addressed the issues described above.
In the first study by Tang L, et al (Br J Anaesth. 2012 Apr;108(4):623-9. doi: 10.1093/bja/aer501. Epub 2012 Feb 5.) titled “Reduced cerebral oxygen saturation during thoracic surgery predicts early postoperative cognitive dysfunction.” studied seventy-six patients undergoing thoracic surgery with single-lung ventilation (SLV) of an expected duration of >45 min were enrolled. Monitoring consisted of standard clinical parameters and absolute oximetry (S(ct)O(2)). The Mini-Mental State Exam (MMSE) test was used to assess cognitive function before operation and at 3 and 24 h after operation. In this study, the authors found that postoperative cognitive dysfunction correlated with reduced cerebral oxygenation during surgery
Click here to read the abstract of the original work.
A similar study by Suehiro K. et al found similar results. The study titled “Duration of cerebral desaturation time during single-lung ventilation correlates with mini mental state examination score.” published in J Anesth. 2011 Jun;25(3):345-9. doi: 10.1007/s00540-011-1136-1. Epub 2011 Apr 12. looked at “Sixty-nine patients , each of whom received combined thoracic epidural and general anesthesia. rSO(2) was measured using INVOS 5100 (Somanetics, Troy, MI, USA) before anesthesia (baseline value) and until SLV was completed. Patient cognitive function was assessed using the mini mental state examination (MMSE) on the day before surgery (baseline) and then repeated 4 days after surgery. The patients were classified into two groups: with (desaturation group, group D) and without (nondesaturation group, group N) cerebral desaturation during SLV. Cerebral desaturation was defined as a reduction of rSO(2) during SLV less than 80% of the baseline value.” They found that the duration of cerebral desaturation correlated with postoperative cognitive dysfunction.
Click here to read the abstract of the original work
Cerebral oxymetry is becoming increasingly available and should be considered for the elderly patient scheduled for one lung ventilaion.