Driven to Drink?
Driven to Drink?
The 6:30 a.m. drive-through line is long but the beverage baristas inside have got the gig down. Take the order, take the money, write on the cup, hand it off and move’em forward. Just across the overpass to our medical center, Starbucks customers line up bumper to bumper on their way to work. And another of the Seattle-based ‘bucks right inside the entrance to the med center picks up the slack. Mmmmm, creamy, sweet, warm…what’s not to like about lapping up your favorite frap on the way to tackling a heavy work schedule? Answer: The heavy part. Beverages are making us fat.
Getting Juiced
Let’s start with juice. Orange juice and the members of its expanding family, are loaded with sugar. They may be fortified with vitamin C, added calcium, or may contain those magical anti-oxidants that didn’t make it into your lunch bag, but most juices are also fortified with sugar, frequently over 15 grams of sugar per 8-ounce serving. An 8-ounce glass of Tropicana original orange juice has 114 calories. 70 calories are sugar and though it may satisfy 96% of your daily requirement for vitamin C, there is only a tad of added calcium and a smaller tad of vitamin A. Ounce for bounce, the payoff isn’t there. A fresh orange, however, has a much lower 62 calories of which 48 are natural sugar(fructose), and it provides 116% of your necessary vitamin C. An orange supplies twice the natural calcium as juice, three times the vitamin A plus 3.1 grams of natural fiber. Plus, you get to chew!
There are entire aisles devoted to fruit- flavored beverages in bottles, boxes and cans in your shiny, upscale grocery chain, but nothing satisfies your body’s needs like fresh, whole fruit, the more color and the more variety, the better. If ya just hafta have your bananas and berries in a beverage, get out the blender and give it a whirl. You won’t need to sweeten the pot.
Smooth Move
Blenders are used for making the smoothie. Originally, the smoothie was a fruit and ice beverage, sometimes with added sugar. Although it debuted as a beverage in the 1930’s, Wikipedia says that the term smoothie/smoothy was actually conjured up by the hippies, though I don’t remember seeing any at Woodstock, and that California, with its ready access to fresh seasonal fruit was the original venue for vending it. Now we blend smoothies choosing from yogurt, protein powder, kale, carrots, blueberries, strawberries, milk…the list is endless but the calories are increasing with the options. It isn’t difficult to find a smoothie shop right around the corner from your produce market, only you’ll drink close to 300 calories if you buy it already made. Go back around the corner, concoct your own smoothie and you take control. To get through a busy day in the OR and still get your nutrients, a smoothie is a great choice. Opt for low fat, no sugar-added, skimmed-milk, light yogurt or water-based, make either fruit or veggie drinks, and avoid expensive, high-calorie add-ins. If your smoothie is meant to enhance your work-out, a tablespoon of protein powder is a fine idea. If dessert is a smoothie, go back to the original 1930’s recipe by using simply fresh fruit and ice. Eliminate the sugar and pour it in a six-ounce wine glass. Now that’s a juice bar!
Are You a Soda Jerk?
Coke, 7-up, Pepsi, Dr. Pepper, Sprite, Mountain Dew, Orange/Strawberry/Grape/Teenage Crush(just checking to see if you’re reading closely), Cream soda and Root Beer are just a few of today’s and yesterday’s beverages-that-make-you-belch. For some reason, we get a kick out of slugging down that nutrient-free, sweet, fizzy bev and emitting a healthy g-blurp! within seconds after downing the drink. But colas do not satisfy thirst. They are wet and sometimes wild, but the ingredients are more de-hydrating than satisfying. If you choose a caffeine-loaded, high-sugar cola bathed in dark dyes, you are headed for more thirst after drinking than before. And you just slurped up at least 96 calories per 8 ounces. A 12-ounce Classic coke is 144 calories and the same fluid measurement of Pepsi or Dr. Pepper weighs in equally at 150. Don’t forget, there’s sodium in them thar streams of sugar and diet sodas have even more. When you just want a little something sweet, a clear soda is the better choice, and a tall, glass, glass of iced cold water is best of all.
The Buzz
Alcoholic beverages are a whole other fast track to fat. We try to jump-start the day with coffee; we imagine we’re getting a nutrient-dense kick with juice; we substitute meals and assume we’re enhancing exercise with smoothies; we pretend to quench our thirst with sodas; but there’s no denying the reason for consuming that 16-ounce margarita or two 6-ounce glasses of Menage e Trois…red or white. It’s recreation. Recreational drinking isn’t a sin, but be aware and compare. One 4-6 ounce glass of red wine is typically 120-150 calories, no worse than a large serving of crunchy, sweet, juicy, red seedless grapes full of fiber and dessert-like qualities, but hey, I only said, “Be aware!” White wine, though lower than red in calories by 25%, does not supply the same number of nutrients as red wine, obviously. Think spinach and mushrooms, dark and light. But neither red nor white is great for metabolizing fat… it’s alcohol, after all. You’ll still need to drink plenty of water and skip the sucrose to avoid those heart-pounding chest rhythms. And do you really want your morning mouth to feel like a cardboard balloon?
Hard liquors are worse for you than wine. If you insist on preserving your right to imbibe the hard stuff, keep these things in mind. On a regular diet of hard drink, Your tummy will get soft fast and your red nose may qualify for holiday hire. Above the others in calories ounce for ounce, more toxic to your internal organs, completely free of nutrients, and potentially more addictive than adult beverages with lower alcoholic content, hard stuff is a poor choice all the way around. Particularly if you are on a wellness program that includes weight loss, deep six the Ten.
There are those who think that a nice cold one quenches the thirst after a nice hot one. It doesn’t. You will not cool down by drinking two pints of Fat Tire after mowing the yard or after playing baseball for two hours. But you can get a fat tire. Beer does not re-hydrate; it doesn’t even hydrate; it is not a substitute for water. What’s not to understand? And if you have any interest at all in a flat tummy, fresh, sweet breath, skin that isn’t sticky and smelly and sweaty at bedtime, and if you’d like less opportunity to make a fool of yourself during Sunday afternoon’s TV Testosteronathan, then load up on water before watching the game, drink at least a quart before playing in one, and don’t touch a beer after mowing until you’ve fully re-hydrated with agua fria. That beer-belly syndrome? It’s nasty-looking, it’s high-risk and it’s for real. Try Sparks.
Be-hold!
Here’s a last word about the extent to which industry here in the States has embraced the beverage boom. Behold the cup holder! We are so dependent on doing something with our hands that nothing with wheels passes market inspection unless it sports a holder for a cup. Nothing with wheels is exempt. There’s a cup holder in your car, your truck, your child’s stroller, your grocery cart, your golf cart, your bicycle(okay, safety issue, fair enough), your yard wagon, your oversized cooler, your computer bag, your rolling backpack, your commercial bus, train or plane tray, and your beach roller bag, not to mention purses, fanny packs, exercise belts, cardboard drink holders…the list is endless, but not surprising, at least in the USA. In Germany, a Bavarian Motorwerks standard issue comes cup-free, but in Spartanburg, SC, BMW assembles the high-end European parts and adds cupholders, “nur fuer uns!”
You Can Lead a Person to Water, but Can You Make ‘em Think?
When you are offered “something to drink,” do you think coffee, water, or a shot of Jack?
Okay, so that may depend on what kind of day you’ve had in the OR and whether it’s
6:00 a.m. or p.m., but, truthfully, if you are a two-fisted cola consumer, a caffeine dependent addict, a juice bar fly, or a regular consumer at Friday Nights Live, it may be time to balance your beverage accounts. Click on some of the links below to read some nutrition facts and beverage tips’info. Start thinking about what, why, and how much you drink BEFORE you drink it. A flat tire is a lot easier to fix than a fat one. Prost!
Compare the Keurig Chai Latte to the Starbucks Frappuccino
Click here for Smoothies
How many calories in a glass of wine? Click here
How many calories in a non-alcoholic beer? Click here
What drinks cause dehydration? Click here
The truth about green tea…Click here
Please visit Liz at www.bdyfrm.com to read the daily Lizlines and Friday Lizlimerick. Discover
Liz’s Bands In The Park mobile browser, a perfect companion for your walking or running group.
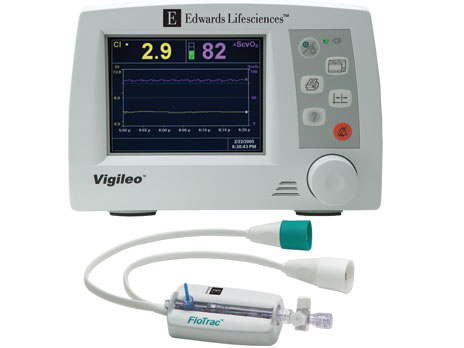
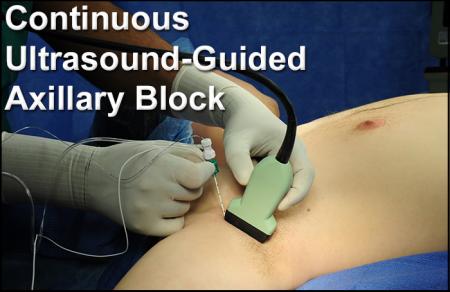
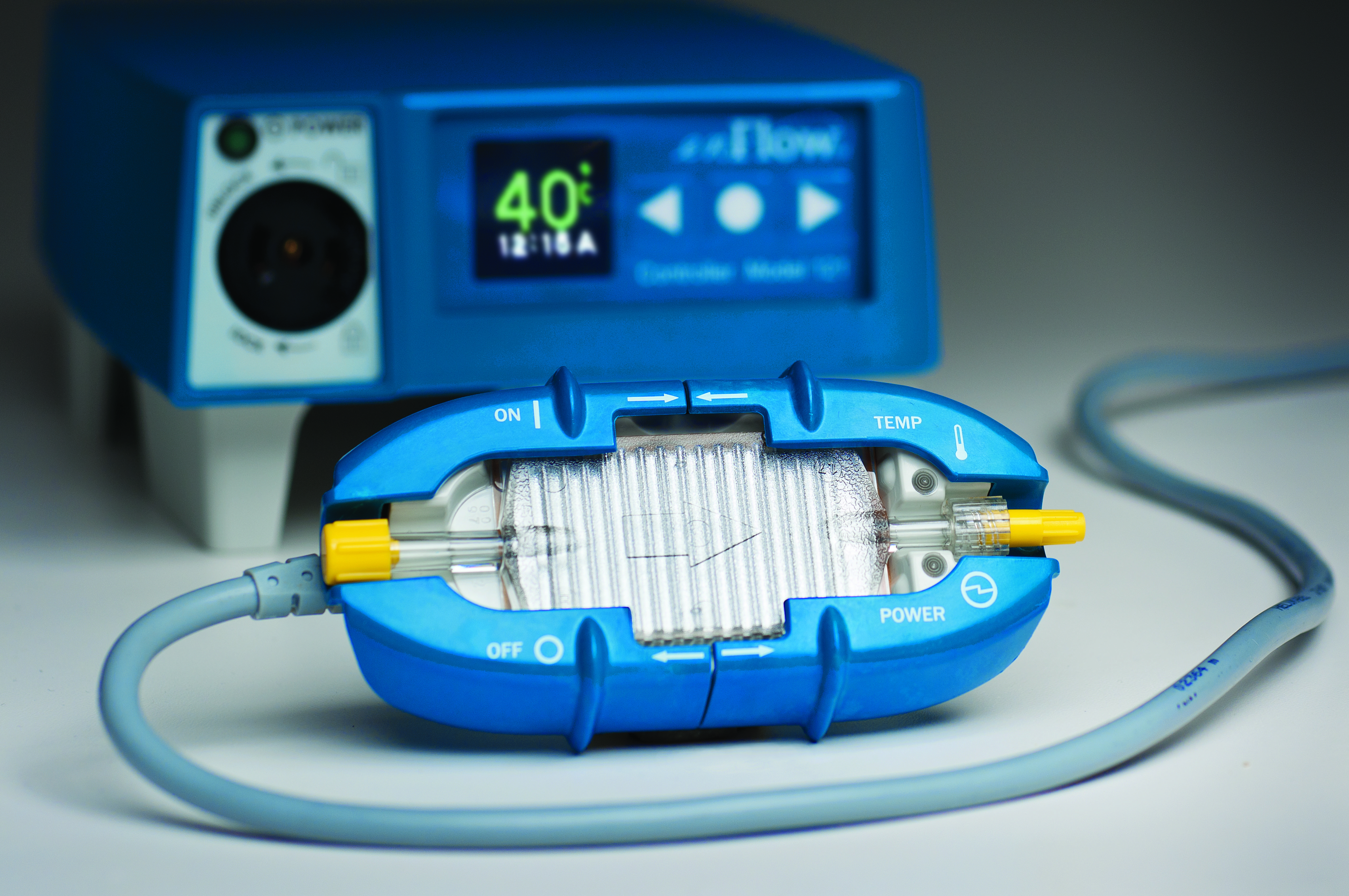
 In the era of Healthcare reform, the practice of anesthesia is being redefined by both the advancement of technology and the impact of regulations. As the scope of anesthesia care emerges from the head of the table to include care across the entire perioperative course, the anesthesia team must evolve to meet the new demands.
In the era of Healthcare reform, the practice of anesthesia is being redefined by both the advancement of technology and the impact of regulations. As the scope of anesthesia care emerges from the head of the table to include care across the entire perioperative course, the anesthesia team must evolve to meet the new demands.