The Circuit Train
Working out can be whole lot simpler when you know the drill! If you need one day a week to “relax your mind” while actually getting your work-out, try circuit-training. There are several good things about using an established circuit and here’s just one. You can go get a member of the training staff for a free orientation around the circuit. Reservations encouraged.
 A circuit provides a moderate level work-out and consists of gym-level machines set up in a circle, a neat little rectangle or at the very least, all on the same side of the gym. If they are not grouped, it’s not a simple circuit, it’s a hairy maze. There will be one or two machines for each specific muscle group and in a well-thought-out arrangement, muscles will be grouped to keep you in order. Remember? It’s 4:30 a.m. before a 12-hour day of one heart, two gall bladders and whatever last-minute trauma is scheduled and you’re looking for a straight-forward work-out, not discombobulation. Start with shoulders and begin working your way around the circuit.
A circuit provides a moderate level work-out and consists of gym-level machines set up in a circle, a neat little rectangle or at the very least, all on the same side of the gym. If they are not grouped, it’s not a simple circuit, it’s a hairy maze. There will be one or two machines for each specific muscle group and in a well-thought-out arrangement, muscles will be grouped to keep you in order. Remember? It’s 4:30 a.m. before a 12-hour day of one heart, two gall bladders and whatever last-minute trauma is scheduled and you’re looking for a straight-forward work-out, not discombobulation. Start with shoulders and begin working your way around the circuit.
Overhead Shoulder Press and perhaps Incline Shoulder Press will be your starting place. If you’ve not had the orientation, you’ll need to read the instructions printed on one of the supporting braces of the press. Adjust the weight plates, adjust the seat front-to-back and up or down, sit with “Body Firm” posture, use an overhand grip and press the contraption overhead(or angled up and outward) until fully extended. Voila! Rest 30 seconds between one or two more “sets” or press onward.
Note: Adjusting the set-up options correctly and appropriately is tantamount to getting the most out of each exercise, but even more importantly, to remaining uninjured. Too much weight can crash back down, hunching shoulders can pinch your neck, exhaling at the wrong time can challenge your heart(and not in a good way), and failing to use your abs will arch and injure your back. Use caution and common sense. You too, Men!
Chest Press and Seated Chest Flies will be next and, once again, read the instructions, adjust all of the set-up options – front to back, seat up or down, weight plates – and be seated. When seated, your feet should be flat on the floor unless there are little angled platforms for your feet. Both of these machines are harder than you think so err on the side of caution and keep it light until you’ve found the level of exertion that challenges without causing pain.
Seated Lat Flies are the reverse of Seated Chest Flies – not to be confused with seated front flies which require elbows bent and arms to open and close like French doors – and may be part of the same machine. To work the chest, you’ll face outward; to work the back, you’ll face inward. And the Seated Lat Row, which has three set-up adjustments, should be next.
These require feet flat on the floor, not tucked behind you so you fall forward, nor extended in front so you can row your boat. You’re not in an outrigger canoe in Hawaii. You’re in the gym, darn it, at 4:30, darn it, before doing a heart, darn it…feet flat on the floor, please.
Triceps and biceps are next on the circuit. Note the work-out moving from strong shoulder exercises, to large chest and back muscles, to the smaller, but potentially so down-right gorgeous tri-bi muscles, the ones that never show in the OR but show big time on a beach…in Hawaii. You can see what’s on my mind in February! Biceps will be a standard Seated Biceps Curl and/or a Preacher Curl. I don’t get why this is called “preacher” but google says it’s because the arm position resembles someone praying. You’ll actually look like someone holding a Bible or a hymnal a whole lot more than praying, but whatever floats your boat is what you should visualize. Just do it! Remember, the key to good biceps curls and triceps curls is the anchoring of the elbow and maintaining neutral wrists. Curl is the basic motion, not the rolling and bending of the wrist to avoid effort.
Legs are next and last. Expect to do Seated – or angled supine – Adduction and Abduction as well as Seated Leg Extensions and maybe Leg Curls. You’re a lucky little guy if there is also a Seated Calf Raise and a Leg Press. A circuit is not generally meant to challenge to the extent or even in the same way as a full-blown 45-set work-out, so three leg machines are really enough. Lunges and squats are “on on your honor.” Crunches can wait.
Okay, you’re done. But if you did only one set of the circuit, take a 60-second break, not a 5-minute text conversation with your broker, and do the circuit again. People tend to monopolize equipment at the gym, especially cardio equipment, but the circuit may be popular, too. So you may just want to claim each machine in its turn and hang onto it until you’ve completed your two or three sets of each. Then when your legs are finished – and they WILL be – you can wobble in and out of the shower, hide your coif under a scrub cap, and take a non-circuitous route to the hospital without looking back.
To learn more about exercising with safe, efficient form, visit Liz at www.bdyfrm.com.
Read Lizlines and the weekly Lizlimerick posted Monday through Friday every week of the year.
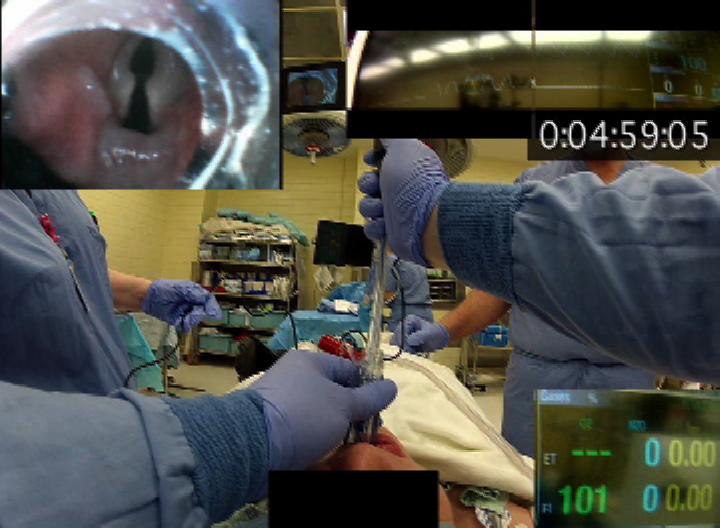
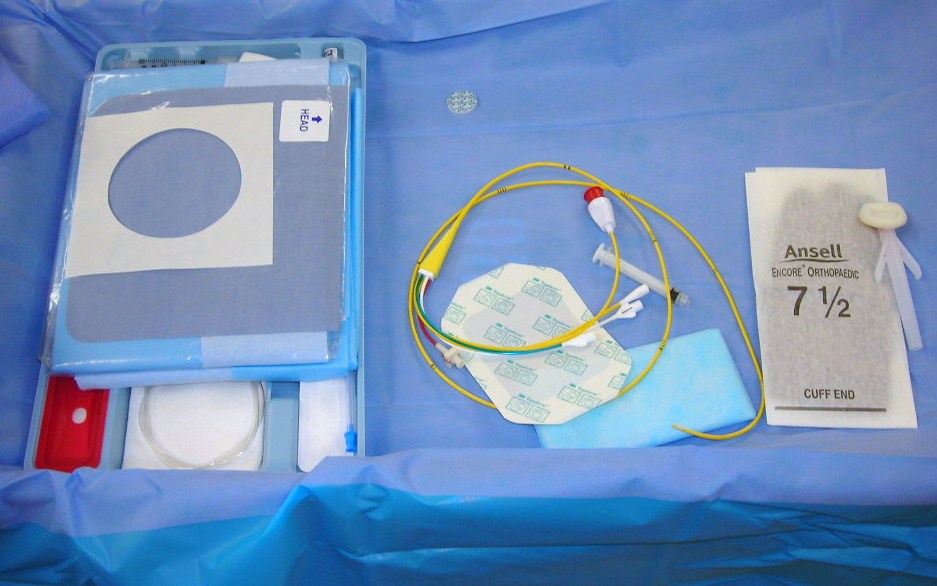
 Automated Anesthesia Recordkeeping (AARK) has been available for over 20 years and is being used in more and more operating rooms across America and around the world. Despite becoming mainstream technology, AARK continues to generate controversy. Is the advantage of automatic physiologic data capture offset by a loss of vigilence by the anesthesia provider? Several studies have investigated the loss of vigilence related to AARK.
Automated Anesthesia Recordkeeping (AARK) has been available for over 20 years and is being used in more and more operating rooms across America and around the world. Despite becoming mainstream technology, AARK continues to generate controversy. Is the advantage of automatic physiologic data capture offset by a loss of vigilence by the anesthesia provider? Several studies have investigated the loss of vigilence related to AARK.