Same Song Different Verse – If It Wasn’t Documented…..
 Consider for a moment, that you or a colleague is facing legal action that, on the face of things, appears absurd. How absurd? Well, think for a moment about the first time that you learned how to place an intravenous (IV) line. The first thing that you were taught to do (after determining the correct patient, catheter size, and limb selection) was – clean the site. Traditionally we used alcohol either provided in an IV start kit or provided by our facility. How many of us thought about, or consulted the relevant science, regarding which preparation solution was actually better for patient care?
Consider for a moment, that you or a colleague is facing legal action that, on the face of things, appears absurd. How absurd? Well, think for a moment about the first time that you learned how to place an intravenous (IV) line. The first thing that you were taught to do (after determining the correct patient, catheter size, and limb selection) was – clean the site. Traditionally we used alcohol either provided in an IV start kit or provided by our facility. How many of us thought about, or consulted the relevant science, regarding which preparation solution was actually better for patient care?
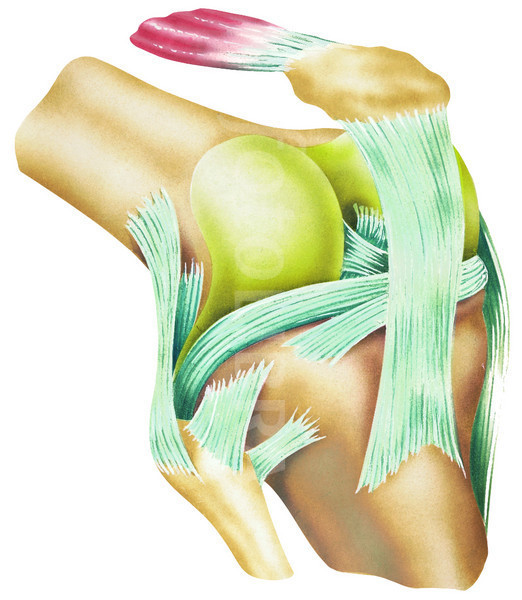
Now lets take it up notch. Consider what you do as an anesthesia provider when you are preparing to place an epidural catheter or a subarachnoid block. Most of the kits that we used in school and current practice have supplied within them a skin cleansing preparation. According to one manufacturer, B. Braun (bbraunusa.com/images/bbraun_usa/bbrauncatalog.pdf; F3), the supplied cleaning preparation in standard single dose epidural trays is povidone iodine. Again, how many of us question the skin preparation solution provided in a kit by a manufacturer that our facility has chosen to select for us? Relevant science indicates that a better skin preparation solution for neuraxial blocks is chlorhexidine. Furthermore, this solution is optimal when used from a single use package, instead of poured from a multi-use container.
What is the importance of such minutiae? Well, suppose a post-partum patient presented to the ER 4 days after discharge from the mother-baby unit of Smallville Community Hospital with the following symptoms: low grade fever, back ache, intermittent weakness of the right lower extremity. During her ER workup, the on call anesthesiologist, Dr. Nurves, is consulted since the patient had an epidural for labor analgesia. After his physical exam, Dr. Nurves suspects the patient has an epidural abscess. He orders an MRI that confirms his suspicions. Now fast forward 18 months. The patient decides to file a claim against her anesthesia providers for causing the pain and disability from which she now suffers. She suspects her current problems are from the epidural abscess…….
When an attorney is tasked to evaluate this type of claim, the attorney will seek a healthcare professional who is familiar with the standards of care surrounding the activities related the client’s labor epidural for analgesia. Imagine the professional conundrum provided by the following clause on the anesthesia record “Sterile prep and drape” without further elaboration. Would it make any difference if we added another detail: the epidural was placed by a trainee (either physician or nurse) and the use of the trainee was NOT noted on the anesthesia record. Additionally, the patient, and her spouse, recalls multiple attempts at placing the epidural; this is also not noted on the chart. So how does one determine if standards of customary practice were met in such a situation? The use of the trainee, and the multiple attempts at placing the epidural catheter are not documented in the records. These items are not facts in evidence. It is a fact however, that if cultures are obtained from an epidural abscess with bacterium that are not normally found in the epidural space, AND the patient’s physical exam prior to the placement of the epidural does not specifically indicate a bacterial infection in the area where the epidural catheter was to be placed AND (perhaps most importantly to us) the modality for transmission of bacterium into the epidural space is under the exclusive control of the anesthesia provider, then supporting data can be introduced to create a scenario whereby the anesthesia providers who placed the epidural catheter caused the epidural abscess AND the related sequela. What type of supporting data? Standards of care regarding neuraxial blockade; sterile skin preparation; and care documentation. Documents of professional standards, along with several peer- reviewed clinical reports regarding sterile skin preparation are readily available in any medical library (electronic or traditional) or via the world wide web.
A well researched review providing the who, what, when, where, and why of how we are supposed to practice our craft can speak volumes to a trier of fact (a judge or a jury) as to whether or not a patient’s claim has merit. So what is the take home message: Know and adhere to your professional standards of care (review them if necessary) and keep up with the state of your science.
Pamela Chambers, MSN, CRNA, EJD
www.lexterraeconsulting.com
References
Barash, P.G., Cullen, B.F., & Stoelting, R.K. Clinical Anesthesia 3rd Ed. Ch 26 Epidual and Spinal Anesthesia p 651 Lippincott Raven, New York 1997
Birnbach D.J. et al, Povidone Iodine and skin disinfection before initiation of epidural anesthesia. Anesthesiology. 1998; 88:668-672
Nagelhout, J. J., Zaglaniczny, K.L. Nurse Anesthesia 3rd Ed. Ch 44 Obstetric Anesthesia p 1066 Elsevier Saunders, St. Louis 2005
Stoelting, R. K., Miller, R.D. Basics of Anesthesia 3rd Ed., Ch. 12 Spinal and Epidural Anesthesia p 173, Churchill Livingstone, New York. 1994
Pamela Chambers, MSN, CRNA, EJD
www.lexterraeconsulting.com