 The clinical anesthetist is frequently challenged with the critically ill patient presenting for non-cardiac surgery. Often, they are in a weakened condition with very little physiologic reserve. It is essential that fluid administration is goal directed to optimize outcome. In this patient population, hypovolemia will lead to hypotension and related complications. However, excessive fluid administration will lead to heart failure. Therefore, fluid optimization is essential in the critically ill patient.
The clinical anesthetist is frequently challenged with the critically ill patient presenting for non-cardiac surgery. Often, they are in a weakened condition with very little physiologic reserve. It is essential that fluid administration is goal directed to optimize outcome. In this patient population, hypovolemia will lead to hypotension and related complications. However, excessive fluid administration will lead to heart failure. Therefore, fluid optimization is essential in the critically ill patient.
An essay published by the Edwards Company “Using Fluid Optimization to Improve Hemodynamics : FloTrac Sensor” makes the following statement:
- Successful fluid optimization has been shown in numerous clinical studies to lead to improved patient outcomes, including reduced morbidity and shorter hospital stays
- The studies are typically based on the physiological principles outlined by the Frank-Starling curve, which states that an increase in preload or volume will lead to cardiac flow-related improvement (e.g., better stroke volume) up to a certain point, after which the “law of diminishing returns” applies.
The essay goes on to state that there are 3 ways to assess fluid status:
- Stroke Volume Variation (SVV): For control-ventilated patients, SVV has been proven to be a highlysensitive and specific indicator for preload responsiveness. As a dynamic parameter, SVV has the advantage of predicting whether a patient will benefit from volume before the fluid is given.
- Passive Leg Raising (PLR): In situations where it is not possible to use SVV (i.e., during arrhythmias, when patients are not on control-mode of ventilation, or in patients at risk of complications from fluid loading), simply raising the legs has been proven clinically to act like a “self volume challenge” to indicate the patient’s status on the Frank-Starling curve. If the patient is fluid-responsive, SV will increase substantially.
- SV Fluid Challenge: In the rare case when neither SVV nor PLR is feasible, the FloTrac system provides a highly efficient method for assessing fluid responsiveness via a standard fluid challenge. The administration of a small volume of fluid (e.g., 250-500 mL) and observance of the corresponding change in SV and/or CO can indicate whether further volume will improve cardiac performance.
Click here to read the essay
Maxime Cannesson MD, University of California, Irvine has published a full lecture complete with slides detailing the importance of goal directed fluid therapy during the intraoperative period. The lecture may be viewed on Youtube and will give the viewer a foundational understanding of optimizing fluid therapy. Click here to view the video.
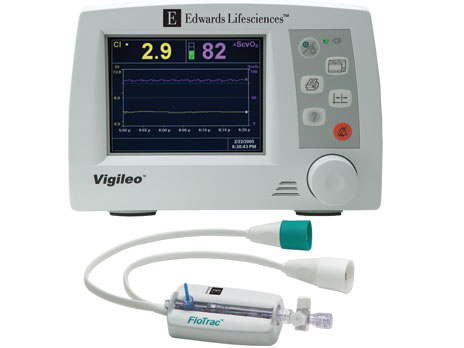
To assist the anesthetist with goal directed fluid therapy, the Edwards Lifesciences Corporation has introduced the FloTrac Sensor and Vigileo monitor to clinical practice. These devices help the anesthetist to evaluate the patient’s fluid status with respect to the Frank Starling curve and make appropriate goal directed decisions with relation to fluid administration
Click here to go to the Edwards web site and learn about the FloTrac sensor and Vigileo monitor.
PROCRNA.COM would like to hear from anesthetists with experience using the Vigileo monitor. Please read the articles, view the video and return to share your comments with your colleagues.
My facility (UC Davis Medical Center) has used the vigileo since inception. As a group we use the vigileo for goal directed fluid therapy. I have used much less fluid since and use more colloid than IV fluid in the past. Limitations are usually related to dysrhythmias and boluses of pressors. However, even with those limitations, trends can be followed even if the actual SVV number is inaccurate. The surgeons are impressed with the postop results and encourage its use.