Building Common Purpose
This is the third in a series of blog articles applying political quotes to frontline leadership. Previous articles have applied the words of Hillary Clinton and Mike Pence to frontline healthcare management. There is no intention of supporting or disparaging any candidate or party but rather learning from their words of wisdom. We will have to wait and see whether or not politicians and parties can turn words into action.
“You are the director of your own movie; if you aren’t enjoying what you are doing, change it.” “Stand up for principles and offer a real alternative.” Gary Johnson
 Same stuff, different day. Is that your experience as a frontline leader and manager? Going back a few years, the basic murder mystery was the backbone of evening television. A crime was committed, several suspects were identified, surprise evidence emerged, and the bad guy was caught. The format was predictable, however in 1971 “Columbo” reversed it. A crime was committed with the perp identified up front. Viewers were kept on the edges of their seats while alibis melted away until justice prevailed.
Same stuff, different day. Is that your experience as a frontline leader and manager? Going back a few years, the basic murder mystery was the backbone of evening television. A crime was committed, several suspects were identified, surprise evidence emerged, and the bad guy was caught. The format was predictable, however in 1971 “Columbo” reversed it. A crime was committed with the perp identified up front. Viewers were kept on the edges of their seats while alibis melted away until justice prevailed.
To enable your group to achieve excellence and to keep the job interesting, rewrite your daily script. Engaging your team to edit the script creates a common purpose and becomes the cement that binds the team
Develop a common purpose. If you think you have problems building consensus and motivating a team, consider the challenge faced by Coach Mike Krzyzewski when he agreed to coach the Olympic men’s basketball team. Taking a group of millionaire all-stars and asking them to give up their summer vacations in order to play even more basketball was not an easy task. To be successful, the team needed a common purpose. Coach K took the team to Arlington Cemetery and the tomb of the Unknown Soldier and talked about people giving their lives for their country. He then took the team to the area of the cemetery where recent casualties are buried and they viewed gravestones of people younger than they. He arranged workouts at the military academies where young people were preparing to give all for their country if necessary. When all was done, the team was no longer playing summer basketball; they were playing for the honor of their country and all those who have given their lives to defend it. They had a common purpose.
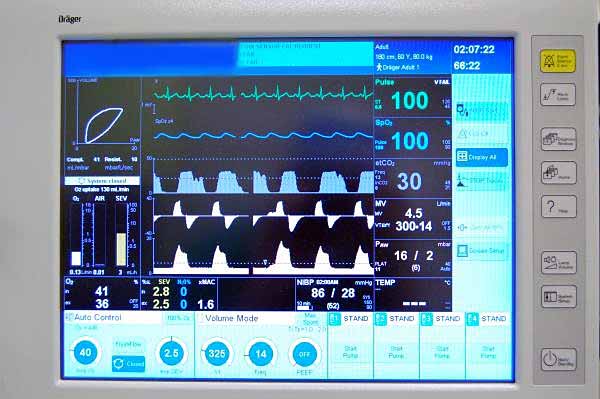
As a frontline healthcare leader, you most likely will not be able to take your workgroup on a field trip to a National monument. Therefore, you must find common purpose within the environment where you live and work.
Create a common purpose
- Focus on patient safety and satisfaction when rewriting the way you conduct your business.
- Openly discuss concerns and explore remedies
- Actively listen to each member of the team as they offer fresh ideas
- Have a former patient or family member talk to your team and tell their story
Change the Script. As a leader, the team looks to you for guidance and wants you to motivate and provide direction. Be bold and confident when interacting with your team. Meet regularly and link the new script to each member personally. Tie common purpose to a sense of urgency and role model the new behavior that is expected of the group
Implement Change
- Display competence and confidence when sharing expectations
- Clearly outline expectations as you role model the desired behavior
- Actively listen to and address concerns of team members. Ask what it would take for them to be fully on board.
- Establish benchmarks to document progress toward achieving the larger goal
- Recognize and reward desired behavior.
Some tasks have to be repetitive, but no one enjoys watching the same movie day after day. As a frontline leader, you will improve the workplace for both patients and workers by making a new script that infuses energy and improves outcome.
Thomas Davis is an experienced clinical anesthetist, leader, speaker and the owner of Frontline Team Development and Leadership.