The application of technology to practice has enabled the CRNA to deliver patient care that is safer and more reliable than at any other time in history. The placement of nerve blocks has always been challenging. Thirty years ago, soliciting paresthesia or trans arterial needle placement were common methods for administering an axillary block. The Ultra sound guided nerve block has increased not only the success rate but also safety to the patient. What can be done to improve on Ultra Sound?
The application of technology to practice has enabled the CRNA to deliver patient care that is safer and more reliable than at any other time in history. The placement of nerve blocks has always been challenging. Thirty years ago, soliciting paresthesia or trans arterial needle placement were common methods for administering an axillary block. The Ultra sound guided nerve block has increased not only the success rate but also safety to the patient. What can be done to improve on Ultra Sound?
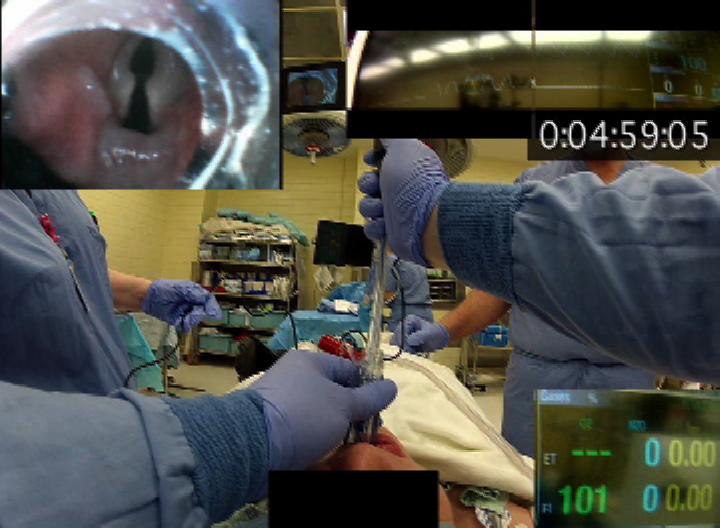
Desjardins AE et al recognized that the success of a nerve block depends upon the proper placement of the needle. They developed a stylet with optical fibers that could collect light for analysis of optical reflectance spectrometry. The theory was that different tissues reflect a different wavelength of light and the stylet could be used to differentiate between nerve and vascular tissues. Click here to read an abstract of their work.
Taking the concept one step further, Balthasar A, et al used the technique on human subjects. They reported that the stylet with optical fibers was able to differentiate between nerve and vascular tissue an on 2 cases detected actual vascular penetration by the needle. Click here to read an abstract of their study.
Will the optical stylet replace ultra sound for nerve block placement? Probably not. However, the addition of the optical stylet which detects penetration of the needle into either vascular or nerve structures could add another element of safety to nerve block placement.